In the early stages of diabetic
retinopathy, our Retina Specialists will
probably just keep
track of how your eyes are doing. Some
people with diabetic retinopathy may
need a
comprehensive dilated eye exam as often
as every 2 to 4 months.
In the early stages of diabetic
retinopathy, our Retina Specialists will
probably just keep
track of how your eyes are doing. Some
people with diabetic retinopathy may
need a
comprehensive dilated eye exam as often
as every 2 to 4 months.
 In later stages, it’s important to start
treatment right away — especially if you
have
changes in your vision. While it won’t
undo any damage to your vision,
treatment can
stop your vision from getting worse.
It’s also important to take steps to
control your
diabetes, blood pressure, and
cholesterol.
In later stages, it’s important to start
treatment right away — especially if you
have
changes in your vision. While it won’t
undo any damage to your vision,
treatment can
stop your vision from getting worse.
It’s also important to take steps to
control your
diabetes, blood pressure, and
cholesterol.
 Injections. Medicines called anti-VEGF
drugs can slow down or reverse diabetic
retinopathy. Other medicines, called
corticosteroids, can also help.
Injections. Medicines called anti-VEGF
drugs can slow down or reverse diabetic
retinopathy. Other medicines, called
corticosteroids, can also help.
 Laser treatment. To reduce swelling in
your retina, eye doctors can use lasers
to make the blood vessels shrink and
stop leaking.
Laser treatment. To reduce swelling in
your retina, eye doctors can use lasers
to make the blood vessels shrink and
stop leaking.
 Eye surgery. If your retina is bleeding
a lot or you have a lot of scars in your
eye,
your eye doctor may recommend a type of
surgery called a vitrectomy.
Eye surgery. If your retina is bleeding
a lot or you have a lot of scars in your
eye,
your eye doctor may recommend a type of
surgery called a vitrectomy.
.jpg)
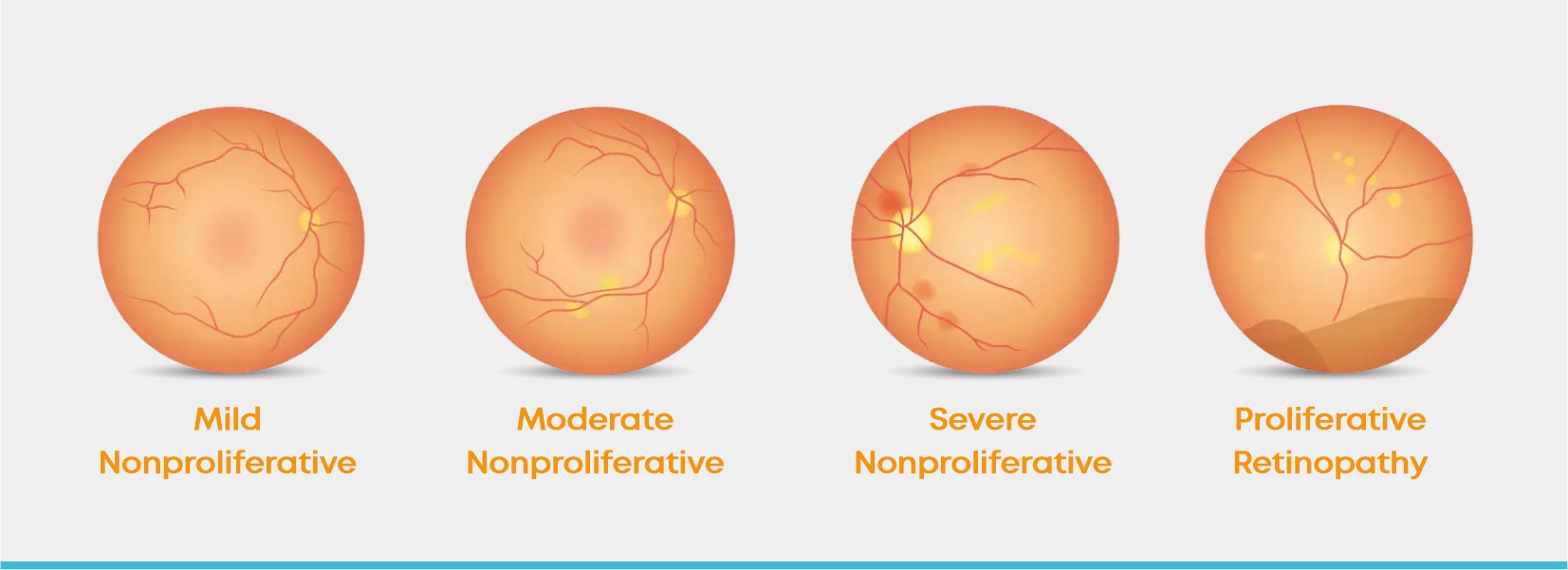
 Diabetic Retinopathy is an eye complication
that occurs in a person due to diabetes and
causes continuous damage to the
light-sensitive tissue at the back of the
eye (the
retina).
Diabetic Retinopathy is an eye complication
that occurs in a person due to diabetes and
causes continuous damage to the
light-sensitive tissue at the back of the
eye (the
retina).